Impact statement
The absence of comprehensive population-based prevalence data remains a significant barrier to informed mental health policy planning and equitable service delivery in Ghana. Our review addresses this gap and offers the first comprehensive synthesis of evidence on the prevalence and social determinants of anxiety and depressive disorders and symptoms among adults in Ghana. We found that over a third of adults may experience anxiety and depressive symptoms. We also identified a range of social determinants of mental health, including demographic, economic, neighbourhood, social and cultural factors associated with prevalence. These findings align with the sustainable development goals and hold implications for the development of both individual-level and population-level interventions. The review also underscores the urgent need to standardise and validate mental health assessment tools, a methodological challenge that extends beyond Ghana to many LMICs. Our findings also contribute to the global discourse on the need for equity-oriented mental health strategies and emphasise the value of locally grounded, yet globally relevant research and practice.
Introduction
Anxiety and depressive disorders among adults are growing public health challenges that significantly contribute to the global burden of disease and disability (Ferrari et al., 2022). Anxiety and depressive disorders adversely impact physical health, quality of life and pose substantial challenges to economic productivity, healthcare systems and societal development (Campion et al., Reference Campion, Javed, Lund, Sartorius, Saxena, Marmot, Allan and Udomratn2022). The burden of anxiety and depressive disorders is particularly pronounced in low- and middle-income countries (LMICs) due to limited financial and human resources within mental health systems (Rathod et al., Reference Rathod, Pinninti, Irfan, Gorczynski, Rathod, Gega and Naeem2017). Examining the prevalence of anxiety and depressive disorders and symptoms, and social determinants of mental health (SDOMH) associated with their occurrence in LMICs such as Ghana, can guide interventions and policy planning.
Recent systematic reviews have found the point prevalence of anxiety and depression symptoms to be 47% and 48%, respectively (Bello et al., Reference Bello, Kannan, Chutiyami, Salihu, Cheong, Miller, Pun, Muhammad, Mahmud, Jalo, Ali, Kolo, Sulaiman, Lawan, Bello, Gambo and Winser2022), and lifetime prevalence to range from 3.3% to 9.8% for anxiety disorders, and 5.7% to 15.8% for depressive disorders across Africa (Greene et al., Reference Greene, Yangchen, Lehner, Sullivan, Pato, McIntosh, Walters, Gouveia, Msefula, Fumo, Sheikh, Stockton, Wainberg and Weissman2021; Bello et al., Reference Bello, Kannan, Chutiyami, Salihu, Cheong, Miller, Pun, Muhammad, Mahmud, Jalo, Ali, Kolo, Sulaiman, Lawan, Bello, Gambo and Winser2022). In sub-Saharan Africa (SSA), the burden of mental disorders is expected to increase by 130% between 2010 and 2050 (Charlson et al., Reference Charlson, Diminic, Lund, Degenhardt and Whiteford2014). This anticipated increase may pose significant challenges for countries such as Ghana, where economic constraints, limited healthcare infrastructure and a shortage of healthcare professionals already hinder the effective treatment of mental disorders. Therefore, interest-holders (e.g., healthcare providers, non-profit organisations, patients, policymakers and researchers) are urging action to address the growing mental health crisis in SSA, including implementing national mental health policies, integrating mental health into primary healthcare, promoting self-care and training formal (nurses) and informal (faith healers and traditional healers) care providers (Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018; Aguwa et al., Reference Aguwa, Carrasco, Odongo and Riblet2023; Sorsdahl et al., Reference Sorsdahl, Petersen, Myers, Zingela, Lund and van der Westhuizen2023). Following the staging model of mental health (Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018), it is important to complement these actions with prevention strategies, targeting SDOMH.
Biological, psychological and social factors influence the onset and progression of anxiety and depressive disorders (Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018). Traditionally, biological and psychological factors have informed psychological and pharmacological intervention development. However, even with optimal access to evidence-based interventions, an estimated 60% of the burden of mental disorders cannot be averted by such interventions alone (Andrews et al., Reference Andrews, Issakidis, Sanderson, Corry and Lapsley2004; Grummitt et al., Reference Grummitt, Barrett, Halladay, Bailey, Birrell, Hunter, Kelly, Champion, Gardner, Nguyen, Chapman, Newton and Teesson2023). Thus, there is a growing emphasis on reducing the burden of mental disorders via SDOMH that may be associated with prevalence and inequities in intervention access (Alegría et al., Reference Alegría, NeMoyer, Falgàs Bagué, Wang and Alvarez2018; Lund et al., Reference Lund, Brooke-Sumner, Baingana, Baron, Breuer, Chandra, Haushofer, Herrman, Jordans, Kieling, Medina-Mora, Morgan, Omigbodun, Tol, Patel and Saxena2018; Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018). SDOMH are largely modifiable, and their impact can be mitigated or leveraged through targeted and universal strategies (e.g., community-based programmes and social policies), to reduce the burden of mental disorders (Rathod et al., Reference Rathod, Pinninti, Irfan, Gorczynski, Rathod, Gega and Naeem2017; Kirkbride et al., Reference Kirkbride, Anglin, Colman, Dykxhoorn, Jones, Patalay, Pitman, Soneson, Steare, Wright and Griffiths2024).
This systematic review focuses on Ghana, a lower-middle-income country with a three-tiered health system that delivers primary, secondary and tertiary care through public, private and faith-based providers (Assan et al., Reference Assan, Takian, Aikins and Akbarisari2018). Over the past two decades, the Government of Ghana has implemented major health and social protection initiatives, including the National Health Insurance Scheme and Livelihood Empowerment Against Poverty programme, to alleviate poverty and improve healthcare access (Otieno et al., Reference Otieno, Angeles, Quiñones, van Halsema, Novignon, Palermo, Palermo, de Groot, Valli, Osei-Akoto, Adamba, Darko, Darko Osei, Dompae, Yaw, Handa, Barrington, Abdoulayi, Angeles, Chakrabarti, Otchere, Akaligaung and Aborigo2022). Mental health has also gained increasing policy attention, particularly with the enactment of the Mental Health Act 846 in 2012, which established the Mental Health Authority to coordinate mental health services and protect the rights of people with mental disorders (Walker and Osei, Reference Walker and Osei2017). The 12-year mental health policy 2019–2030, launched in 2019, further aims to promote mental health, prevent mental disorders and strengthen the management and care of people with mental disorders (Government of Ghana, 2018; Walker and Osei, Reference Walker and Osei2017). Despite these advances, the mental health system in Ghana remains under-resourced and overstretched, with limited funding, workforce shortages, a high treatment gap and severe shortages of psychotropic medication (Asamani et al., Reference Asamani, Ismaila, Plange, Ekey, Ahmed, Chebere, Awoonor-Williams and Nabyonga-Orem2021; Government of Ghana, 2018). The country also performs poorly on indicators of population well-being, such as educational attainment, environmental pollution, gender equality and multidimensional poverty (United Nations Development Programme, 2020).
Ghana is currently experiencing an epidemiological transition, characterised by a double burden of communicable and non-communicable diseases (Government of Ghana, 2018; Otieno et al., Reference Otieno, Angeles, Quiñones, van Halsema, Novignon, Palermo, Palermo, de Groot, Valli, Osei-Akoto, Adamba, Darko, Darko Osei, Dompae, Yaw, Handa, Barrington, Abdoulayi, Angeles, Chakrabarti, Otchere, Akaligaung and Aborigo2022). The World Health Organization (WHO) estimates that about13% of Ghanaians live with a mental disorder (Oppong et al., Reference Oppong, Kretchy, Imbeah and Afrane2016; World Health Organization, 2021). In recent times, the country has faced macroeconomic crises, including a debt crisis, fuel shortages and rising unemployment, which may have increased the risk of mental disorders, including anxiety and depressive disorders, partly by worsening socioeconomic vulnerabilities and amplifying the adverse effects of SDOMH on mental health outcomes (The World Bank Group, 2024). While Ghana is working towards improving mental health care via its 12-year mental health policy (Ae-Ngibise et al., Reference Ae-Ngibise, Sakyi, Adwan-Kamara, Lund and Weobong2023; Government of Ghana, 2018; Mwangi et al., Reference Mwangi, Sakyi, Ae-Ngibise, Lund and Weobong2023), the lack of comprehensive national and local prevalence data for adult mental disorders and insufficient evidence on associated SDOMH hinders efforts to estimate the burden of disease and develop evidence-based multisectoral strategies aimed at improving mental health and well-being of adults in Ghana (Government of Ghana, 2018). Therefore, the primary aims of this review were to (1) examine the prevalence of anxiety and depressive disorders and symptoms among adults in Ghana, and (2) explore SDOMH potentially associated with anxiety and depressive disorders and symptoms. The secondary aim was to examine the prevalence of symptoms of psychological distress among adults in Ghana.
Methods
We followed the Joanna Briggs Institute (JBI) method for systematic reviews of prevalence (Munn et al., Reference Munn, Moola, Lisy, Riitano and Tufanaru2015) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines; see Supplementary Appendix A (Page et al., Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow, Shamseer, Tetzlaff, Akl, Brennan, Chou, Glanville, Grimshaw, Hróbjartsson, Lalu, Li, Loder, Mayo-Wilson, McDonald, Stewart, Thomas, Tricco, Welch, Whiting and Moher2021). We published the review protocol (Awortwe et al., Reference Awortwe, Daivadanam, Adjorlolo, Olsson, Coumoundouros and Woodford2024) and it has been registered in the International Prospective Register of Systematic Reviews (PROSPERO, CRD42023463078). Protocol changes made before analysis are recorded in PROSPERO and reported in Supplementary Appendix B.
Search strategy
We searched nine electronic databases (Supplementary Appendix C) from inception up to September 30, 2024. We manually reviewed the reference lists of included studies and identified systematic reviews by conducting forward citation checks of included studies. We searched grey literature in the Agency for Healthcare Research and Quality, Google Scholar, Health Systems Trust, Open Grey (http://www.opengrey.eu/) and the WHO websites. We contacted researchers and non-governmental organisations working in adult mental health in Ghana to identify unpublished or ongoing studies.
We constructed the search using a combination of Medical Subject Headings and free text words for “mental disorders,” “anxiety disorders and symptoms,” “depressive disorders and symptoms” and “Ghana,” with assistance from a librarian at Uppsala University. The electronic search strategy was peer reviewed by two researchers following the PRESS guidelines (McGowan et al., Reference McGowan, Sampson, Salzwedel, Cogo, Foerster and Lefebvre2016). The PubMed search strategy is shown in Supplementary Appendix C. Search strategies for all electronic databases and the PRESS peer review have been published (Awortwe et al., Reference Awortwe, Daivadanam, Adjorlolo, Olsson, Coumoundouros and Woodford2024). Only studies available in English and Ghanaian languages (e.g., Ewe, Ga and Twi) were eligible.
Eligibility criteria
Eligibility criteria follow CoCoPops (Condition, Context, Population and study design) format:
Condition
Eligible studies assessed anxiety disorders (e.g., generalised anxiety disorder and phobias) and depressive disorders using (1) a structured diagnostic clinical interview following the International Classification of Diseases and Related Health Problems or the Diagnostic and Statistical Manual of Mental disorders; and/or (2) anxiety and depressive symptoms using a validated self-report, clinician or proxy-administered screening tool for anxiety, for example, Beck Anxiety Inventory (BAI) (Beck et al., Reference Beck, Epstein, Brown and Steer1988), and depression, for example, Beck Depression Inventory (BDI) (Beck et al., Reference Beck, Ward, Mendelson, Mock and Erbaugh1961) in an adult sample. There was no restriction on cutoff scores for self-report screening tools due to research suggesting that commonly used standardised cut-offs may not be suitable for adult populations in LMICs (Ali et al., Reference Ali, Ryan and Silva2016; Mughal et al., Reference Mughal, Devadas, Ardman, Levis, Go and Gaynes2020). Studies reporting point, period or lifetime prevalence of anxiety and depressive disorders and symptoms were eligible. Given symptoms of psychological distress encompass symptoms of common mental disorders, such as anxiety and depression in adults (Duarte and Jiménez-Molina, Reference Duarte and Jiménez-Molina2022), the prevalence of symptoms of psychological distress was examined as a secondary outcome. Studies using validated measures, for example, Kessler Psychological Distress Scale (K10) (Kessler et al., Reference Kessler, Andrews, Colpe, Hiripi, Mroczek, Normand, Walters and Zaslavsky2002), to report the prevalence of symptoms of psychological distress in adult samples, were eligible. We excluded studies if prevalence could not be calculated (i.e., symptoms reported only as mean scores) and/or obtained from the study authors.
Context
Eligible studies were conducted in (1) Ghana with adults sampled from the community and/or clinical settings including through online recruitment, or (2) regions that encompass Ghana (e.g., West Africa and SSA) with data on participants living in Ghana that could be extracted or obtained from the study authors. Studies conducted immediately (i.e., <4 months after the official end date) of ethnic and/or political conflicts (e.g., Konkomba-Nanumba conflict and Western Togoland crisis), humanitarian crises or natural disasters were excluded (Lim et al., Reference Lim, Tam, Chudzicka-Czupała, McIntyre, Teopiz, Ho and Ho2022).
Population
Eligible studies included adults (aged ≥18 years). Studies including participants aged <18 years were excluded if they did not present data separately for adults, or if this data could not be obtained via correspondence with study authors. Informed by similar systematic reviews conducted in SSA (Jörns-Presentati et al., Reference Jörns-Presentati, Napp, Dessauvagie, Stein, Jonker, Breet, Charles, Swart, Lahti, Suliman, Jansen, van den Heuvel, Seedat and Groen2021; Bello et al., Reference Bello, Kannan, Chutiyami, Salihu, Cheong, Miller, Pun, Muhammad, Mahmud, Jalo, Ali, Kolo, Sulaiman, Lawan, Bello, Gambo and Winser2022; Kaggwa et al., Reference Kaggwa, Najjuka, Bongomin, Mamun and Griffiths2022; Opio et al., Reference Opio, Munn and Aromataris2022), studies including adults with comorbid physical health conditions were eligible (Austin, Reference Austin2024; Bhattacharya et al., Reference Bhattacharya, Shen and Sambamoorthi2014; Centers for Medicare & Medicaid Services, 2020). Studies focusing on other mental disorders (e.g., personality disorders and psychotic disorders), substance use (e.g., alcohol dependence) and neurological disorders (e.g., multiple sclerosis) were excluded. Studies on prisoners and adults accused of witchcraft were also excluded because these adults are not necessarily representative of the wider Ghanaian population.
Study design
Eligible studies were quantitative and used observational designs, such as longitudinal cohort (baseline data only), case–control and cross-sectional studies. Mixed methods studies were eligible if quantitative data could be extracted or obtained from the study authors. In studies conducted on the same cohort of individuals at the same or different time points, or where samples overlapped, the study with the largest sample and primary outcomes related to this review was included to ensure duplicate data were not included (Opio et al., Reference Opio, Munn and Aromataris2022). Studies reporting secondary data analyses were excluded. Published and unpublished studies were eligible for inclusion.
Study selection
We de-duplicated searches using EndNote V.20 (Clarivate) and imported them into Rayyan for study screening and selection. Title and abstract screening, followed by full paper checks of potentially eligible studies, were conducted independently by two reviewers (F.M. and V.A.). Disagreements were resolved through discussion or consulting a third reviewer (J.W.). Authors were contacted a maximum of two times via email for additional information to determine study eligibility, where necessary. We excluded studies if authors did not respond or provide the requested information.
Data extraction
Data were extracted independently by one reviewer (V.A.) into a standardised Microsoft Excel form (see review protocol) and cross-checked by a second reviewer (F.M. or V.R.).
Quality assessment
Two reviewers (V.A. and F.M.) independently conducted the quality assessment of the included studies using the JBI Critical Appraisal Tool for Prevalence Studies (Munn et al., Reference Munn, Moola, Lisy, Riitano and Tufanaru2015). Each domain was rated as Yes, No, Unclear or Not applicable (Munn et al., Reference Munn, Moola, Lisy, Riitano and Tufanaru2015), with reasons for ratings provided in Supplementary Appendices D and E. The total score ranged from 1 to 9 for individual studies, with the total number of “Yes” scores for individual studies used to appraise studies as low (≤3 points), moderate (4–6 points) or high-quality (≥7 points). Disagreements were resolved by discussion between the two reviewers or by consulting a third reviewer (V.R. or J.W.).
Meta-analysis
We conducted the meta-analysis using Comprehensive Meta-Analysis software V.4. (Borenstein, Reference Borenstein, Hedges, Higgins and Rothstein2022). Individual study data on the point prevalence (i.e., number of cases/sample size) of anxiety disorders and symptoms, depressive disorders and symptoms and symptoms of psychological distress, respectively, were extracted. Data were transformed to their logits to stabilise variances before performing the meta-analysis (Doi and Williams, Reference Doi and Williams2013; Yang et al., Reference Yang, Sun, Nan, Waqas, Nisar, Wang, Rahman and Li2023). We adopted a random-effects model given anticipated heterogeneity across studies. We assessed heterogeneity using Cochran’s Q statistic and measured the proportion of total variability due to between-study heterogeneity using the I 2 statistic. The prediction interval (T 2) was used as an estimate of between-study variance in true effects observed in eligible studies. We performed a sensitivity analysis excluding studies (1) conducted during coronavirus disease 2019 (COVID-19) pandemic, and (2) of lower quality (i.e., quality score ≤ 3), from the analysis to examine whether removal caused any substantial change to overall pooled prevalence estimates. We assessed publication bias using Egger’s regression statistic and funnel plots (Sutton et al., Reference Sutton, Song, Gilbody and Abrams2000) and Duval and Tweedie’s trim-and-fill method to identify and correct for funnel plot asymmetry arising from publication bias (Duval and Tweedie, Reference Duval and Tweedie2000).
Subgroup analysis
We conducted a subgroup analysis to explore sources of heterogeneity and examine the potentially moderating effects of the following factors on prevalence:
-
• Presence of a chronic physical condition (yes/no)
-
• Type of chronic physical conditions (e.g., cancer, diabetes and human immunodeficiency virus [HIV]/acquired immunodeficiency syndrome [AIDS])
-
• Method of assessment (structured clinical interview or screening tool)
-
• Sample size (<384 vs. ≥384)
-
• Study design (case–control study, cross-sectional studies and longitudinal cohort study)
-
• Study quality (low, moderate or high-quality studies)
-
• Time period of data collection (<2020 vs. ≥2020).
-
• Population type (general population vs. specific population). The term “general population” describes adults without distinguishing characteristics related to age, occupation, physical condition or comorbidity, whereas “specific population” describes adults with specific attributes, for example, chronic physical conditions, caregivers, employees, students and older adults (Kaggwa et al., Reference Kaggwa, Najjuka, Bongomin, Mamun and Griffiths2022).
Statistical significance level for subgroup analysis was set at P < 0.05 (two-tailed).
Narrative synthesis
SDOMH potentially associated with anxiety and depressive disorders and symptoms were narratively synthesised, with proximal and distal factors categorised under the demographic, economic, neighbourhood, environmental events, social and cultural domains of the social determinants of mental disorders and sustainable development goals (SDGs) framework (Lund et al., Reference Lund, Brooke-Sumner, Baingana, Baron, Breuer, Chandra, Haushofer, Herrman, Jordans, Kieling, Medina-Mora, Morgan, Omigbodun, Tol, Patel and Saxena2018).
Results
Study selection
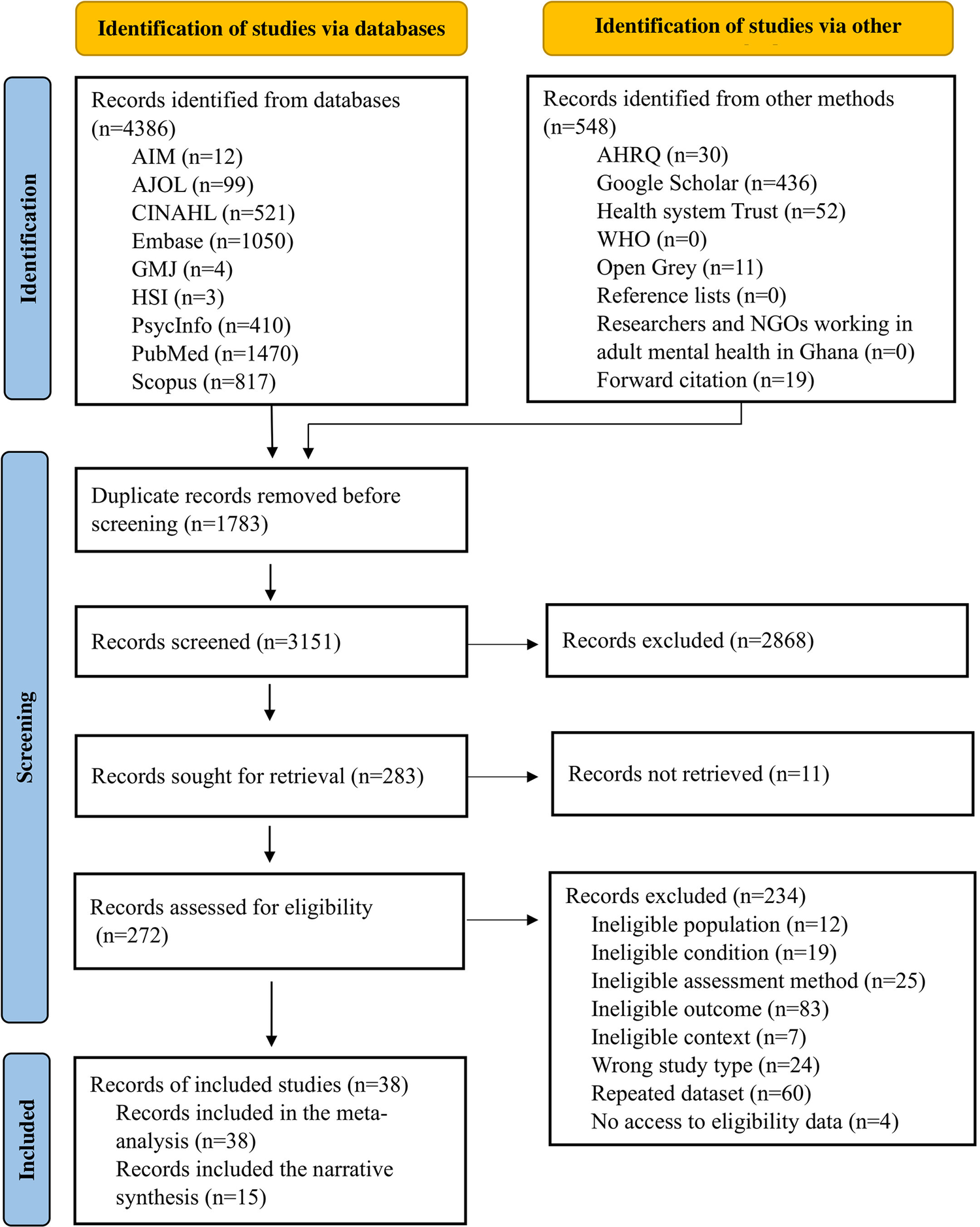
We identified 4,934 records via electronic database searches and other methods. We assessed 272 full-text records for eligibility, of which 38 studies met the inclusion criteria (see Figure 1 and also Supplementary Appendices G and H for detailed reasons for study exclusion).

Figure 1. PRISMA flow diagram of study selection.
Study characteristics and quality
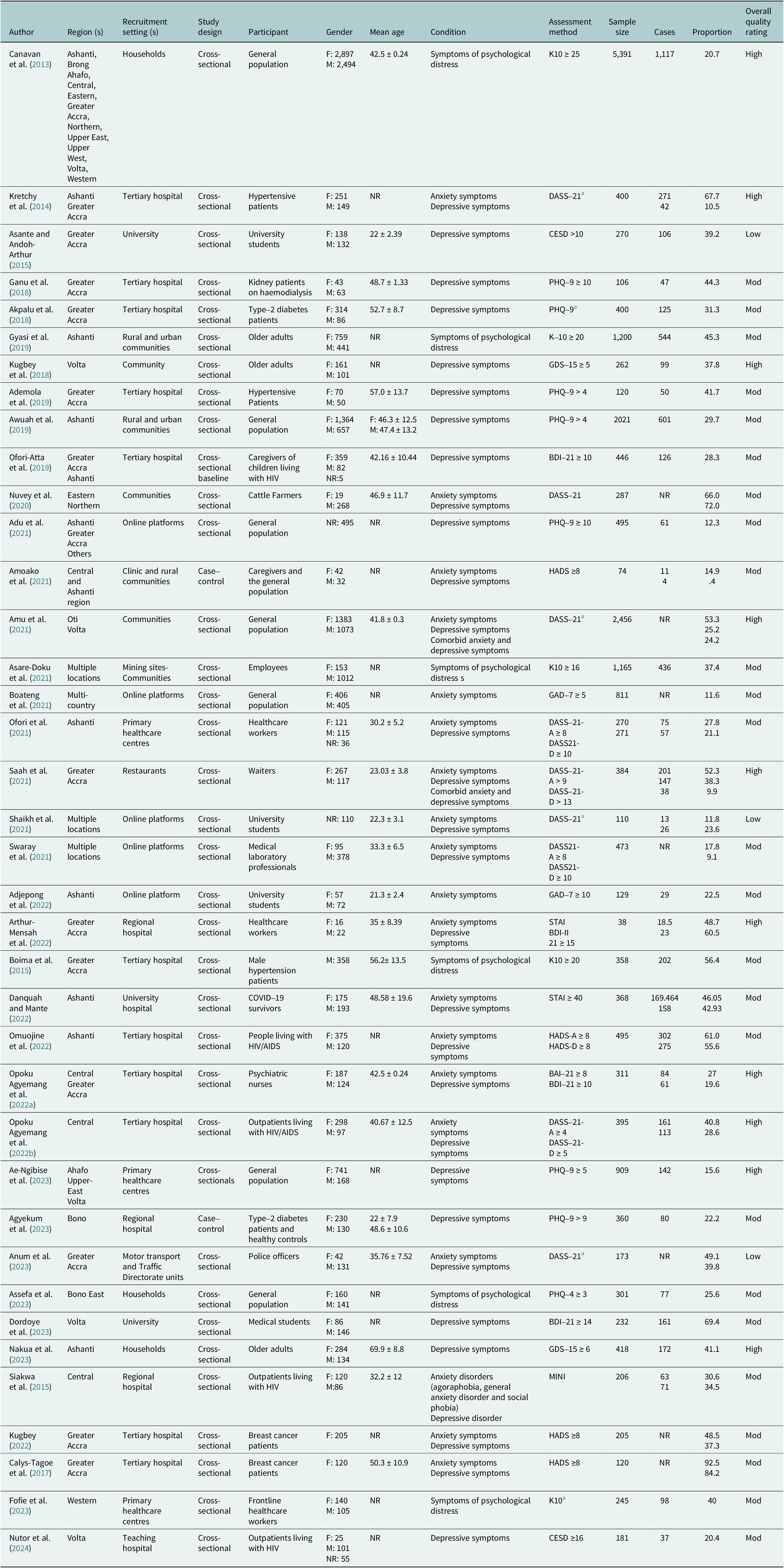
Study characteristics are reported in Table 1. We included 38 studies (N = 22,587 participants – 9,783 males, 12,103 females and 701 whose sex was not specified). Mean age ranged from 21.3 (±2.4) to 69.9 (±8.8) years, and the sample size ranged from 38 to 5,391. Study samples included general populations (7 studies), specific populations (29 studies) and mixed population groups (2 studies). Studies were conducted in community (13 studies), hospital (19 studies), mixed community and hospital (1 study), and online (5 studies) settings. Most studies used cross-sectional designs (35 studies) and were published between 2013 and 2024.
Table 1. Study characteristics and quality assessment

Note: Overall quality rating: Low quality, Mod = moderate quality, high quality.
Abbreviations: NR, not reported; F, females; M, males.
a Cut-offs not reported.
Data on the point prevalence of anxiety disorders and symptoms were reported in 19 studies (N = 7,705). One study assessed the prevalence of agoraphobia, generalised anxiety disorder and social phobia, using the Mini International Neuropsychiatric Interview (MINI) (Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller, Hergueta, Baker and Dunbar1998). The remaining 18 studies assessed the prevalence of anxiety symptoms using self-report screening tools, including the BAI (2 studies), the anxiety subscale of the Depression Anxiety and Stress Scale (DASS-21; 9 studies) (Lovibond and Lovibond, Reference Lovibond and Lovibond1995), the General Anxiety Disorder Scale (GAD-7; 2 studies) (Spitzer et al., Reference Spitzer, Kroenke and Williams1999), the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS; three studies) (Zigmond and Snaith, Reference Zigmond and Snaith1983) and the State–Trait Anxiety Inventory (STAI; two studies) (Spielberger, Reference Spielberger2010).
Data on the point prevalence of depressive disorders and symptoms were reported in 30 studies (N = 12,950). One study assessed the prevalence of major depressive disorder using the MINI. The remaining 29 studies assessed the prevalence of depression symptoms using self-report screening tools, including the first edition of the BDI (3 studies) (Beck et al., Reference Beck, Ward, Mendelson, Mock and Erbaugh1961), second edition of the BDI-II (1 study) (Beck et al., Reference Beck, Brown and Steer1996), Center for Epidemiological Studies-Depression Scale (CESD-10; 2 studies) (Radloff, Reference Radloff1977), the depression subscale of DASS-21 (9 studies), the Geriatric Depression Scale (GDS-15; 2 studies) (Yesavage and Sheikh, Reference Yesavage and Sheikh1986), the depression subscale of the HADS (4 studies) (Zigmond and Snaith, Reference Zigmond and Snaith1983), Patient Health Questionnaire (PHQ-9; 7 studies) (Kroenke et al., Reference Kroenke, Spitzer and Williams2001), and the Zung Self-Rating Depression scale (1 study) (Zung, Reference Zung1965).
Data on the point prevalence of symptoms of psychological distress were reported in 6 studies (N = 8,660). Two instruments, comprising the K10 (5 studies) and the PHQ for Depression and Anxiety (PHQ-4; 1 study) (Kroenke et al., Reference Kroenke, Spitzer, Williams and Löwe2009), were used to assess symptoms of psychological distress.
Quality assessment scores ranged from 1 to 9; most studies were of moderate quality (65.8%, 25 studies, see Supplementary Appendix E). High risk of bias was most frequently identified in domains related to appropriateness of sampling methods (25 studies), adequateness of sample size (14 studies), standard and reliable measurement of condition (28 studies), sufficient coverage of identified sample (16 studies) and, adequateness and appropriate management of response rate (25 studies).
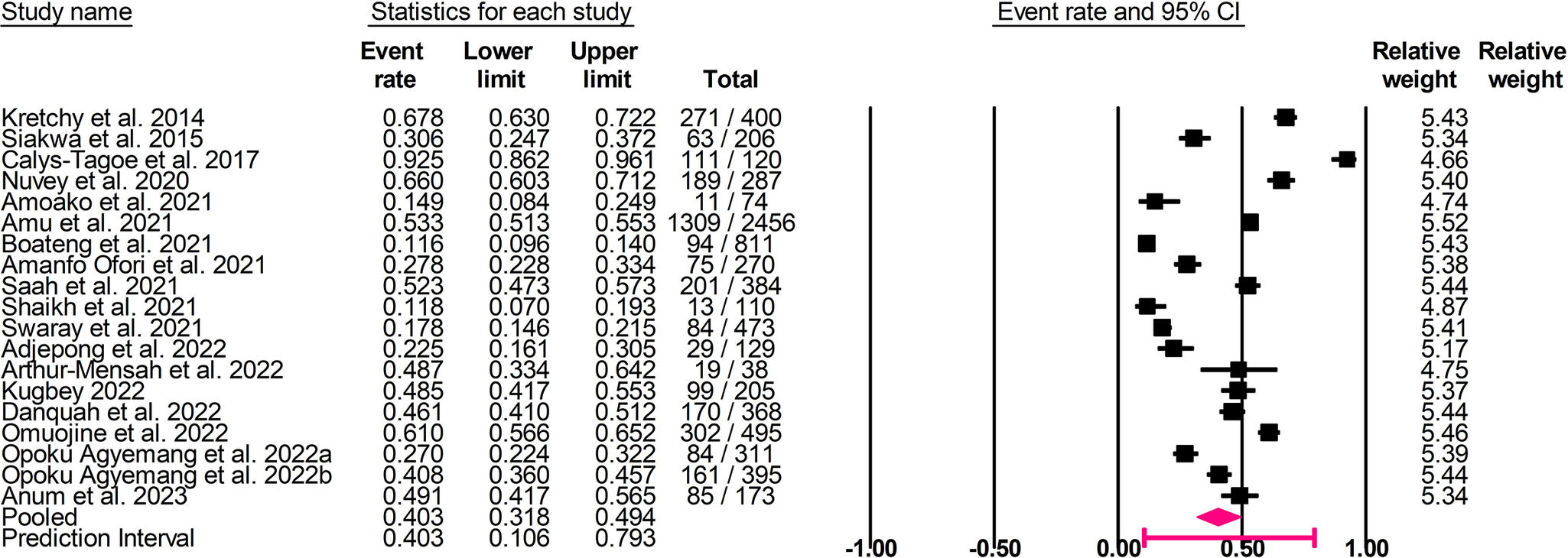
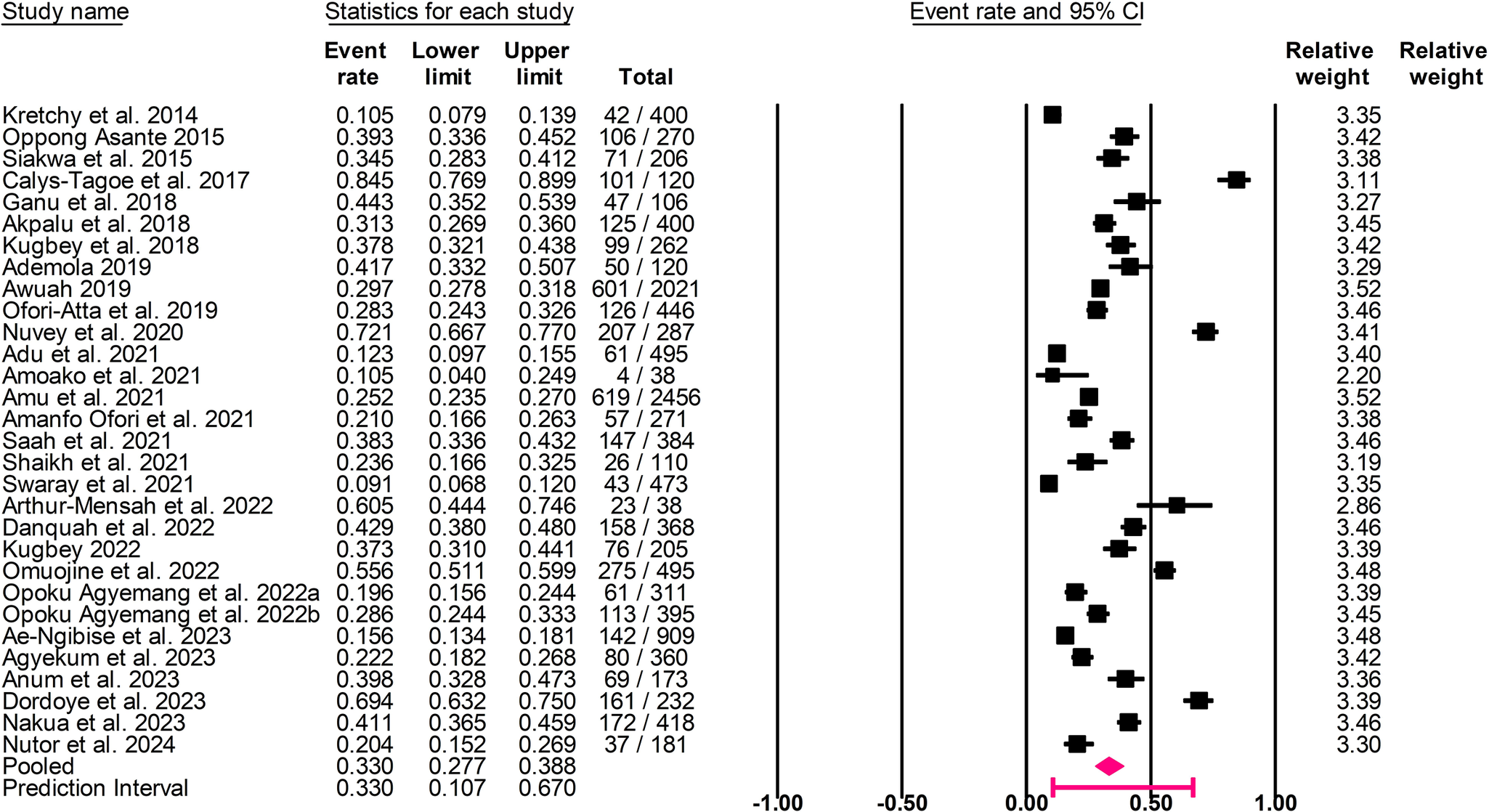
Prevalence of anxiety and depressive disorders and symptoms
The pooled point prevalence of anxiety disorders and symptoms was 40.3% (95% confidence interval [CI]: 31.8–49.4%, I 2 = 98.0%, τ 2 = 0.642, T 2 = 10.6–79.3%; Figure 2). The pooled point prevalence of depressive disorders and symptoms was 33.0% (95% CI: 27.7–38.8%, I 2 = 97.0%, τ 2 = 0.461, T 2 = 10.7–67.0%; Figure 3).

Figure 2. Forest plot of the pooled prevalence of anxiety disorders and symptoms.

Figure 3. Forest plot of the pooled prevalence of depressive disorders and symptoms.
Sensitivity analysis and publication bias
Sensitivity analysis revealed no significant change to the pooled point prevalence of anxiety disorders and symptoms, depressive disorders and symptoms, and symptoms of psychological distress, respectively, after removing studies conducted during COVID-19 pandemic, and studies of lower quality (i.e., quality score ≤ 3) from the analysis via the leave-one-out method.
There was no evidence of publication bias for anxiety disorders and symptoms (Egger’s test, t = 1.42, p = 0.173), depressive disorders and symptoms (Egger’s test, t = 0.83, p = 0.415) and psychological distress (Egger’s test: t = 1.66, p = 0.171). The Duval and Tweedie trim-and-fill analysis suggested imputation of one study to the left of the mean for depression, yielding an adjusted pooled point prevalence estimate of 31.6% (95% CI: 26.3–37.5%). The pooled point prevalence of symptoms of psychological distress was 36.7% (95% CI: 25.2–50.0%, I 2 = 99.0%, τ 2 = 0.456, T 2 = 7.1–81.5%; see Supplementary Appendix J). The Duval and Tweedie trim-and-fill analysis also suggested imputation of three studies to the left of the mean for symptoms of psychological distress, yielding an adjusted pooled point prevalence of 25.2% (95% CI: 16.4–36.7%, see Supplementary Appendix I–K for funnel plots).
Subgroup analyses
Subgroup analysis of the prevalence of anxiety disorders and symptoms
Subgroup analysis showed that the presence of a chronic physical condition (Q = 7.118, p < 0.05), type of chronic physical condition (Q = 9.926, p < 0.05), region (Q = 39.553, p < 0.05) and time period of data collection (Q = 16.568, p < 0.05) were significant moderators of anxiety prevalence (see Supplementary Appendix L). Specifically, point prevalence of anxiety disorders and symptoms was higher in adults with a comorbid chronic physical health condition (59.0%, 95% CI: 42.3–73.8%, 6 studies) than those without it (32.2%, 95% CI: 23.1–42.9%, 13 studies). Point prevalence of anxiety disorders and symptoms was higher in Greater Accra and Ashanti regions (67.8%, 95% CI: 40.1%–86.8%, 1 study), Northern and Eastern regions (66.0%, 95% CI: 38.1–86.0%, 1 study) and Greater Accra region (60.2%, 95% CI: 46.9–72.2%, 5 studies), compared with Ashanti region (38.8%, 95% CI: 26.3–53.1%, 4 studies) and Central region (35.6%, 95% CI: 19.7–55.5%, 2 studies; see Supplementary Appendix M for the regional distribution of prevalence of anxiety disorders and symptoms). Point prevalence estimate of anxiety disorders and symptoms was higher in studies conducted before 2020 (55.8%, 95% CI: 42.6–68.2%, 6 studies) than those conducted from 2020 onwards (26.1%, 95% CI: 18.7–35.2%, 9 studies).
Subgroup analysis of the prevalence of depressive disorders and symptoms
Subgroup analysis showed that population type (Q = 9.426, p < 0.05), region (Q = 39.912, p < 0.05), sample size (Q = 7.219, p < 0.05) and time period of data collection (Q = 12.678, p < 0.05) were significant moderators of depression prevalence (see Supplementary Appendix N). Point prevalence of depressive disorders and symptoms was higher in specific populations (37.7%, 95% CI: 31.6–44.2%, 24 studies) than in the general populations (19.9%, 95% CI: 11.5–32.1%, 4 studies). Point prevalence of depressive disorders and symptoms was higher in Northern and Eastern regions (72.1%, 95% CI: 44.8–89.2%, 1 study) and Greater Accra (46.1%, 95% CI: 36.5%–56.0%, 9 studies), and lower in Ashanti and Central regions (10.5%, 95% CI: 2.5%–35.3%, 1 study; see Supplementary Appendix O on regional distribution of prevalence of depressive disorders and symptoms). Point prevalence of depressive disorders and symptoms was higher in studies with small sample size (39.4%, 95% CI: 32.9–47.9%, 18 studies) than those with large sample size (25.0%, 95% CI: 18.7–32.6%, 12 studies). Point prevalence of depressive disorders and symptoms was higher in studies conducted before 2020 (36.9%, 95% CI: 28.1–46.6%, 10 studies) than those conducted from 2020 onwards (22.6%, 95% CI: 16.4–30.2%, 10 studies).
Social determinants of mental health associated with anxiety symptoms
Seven cross-sectional studies (N = 5,025) reported one or more proximal SDOMH associated with anxiety symptoms (see Table 2). All studies performed multivariable statistical analysis, with adjustment for covariates. None of the studies examined environmental events associated with anxiety symptoms, and SDOMH associated with anxiety disorders.
Table 2. Social determinants of mental health associated with anxiety and depressive symptoms among adults in Ghana (N = 11,248, 15 studies)

Note: X, not reported; AOR, adjusted odds ratio; β, adjusted linear regression model coefficient; CI, confidence interval; OR, odds ratio; *, 95% confidence interval was not reported; **, uncertainties around measure of effects; ***, standard error not reported.
Demographic domain
A total of five studies examined demographic factors that were categorised into three distinct subdomains: age, gender and marital status.
Age
One study found that younger age (i.e., 18–44 years) was associated with higher odds of severe anxiety symptoms (Opoku Agyemang et al., Reference Opoku Agyemang, Ninnoni and Enyan2022a).
Gender
Gender was examined in four studies, all of which reported consistent results. Among these, two studies found that female gender was significantly associated with increased odds of anxiety symptoms (Saah et al., Reference Saah, Amu and Kissah-Korsah2021; Opoku Agyemang et al., Reference Opoku Agyemang, Ninnoni and Enyan2022a). One study found a small but significant effect showing that females had higher odds of experiencing anxiety symptoms than males (Anum et al., Reference Anum, Acquah and Osei-Tutu2023). One study reported that male gender was significantly associated with decreased odds of anxiety symptoms during the COVID-19 pandemic (Boateng et al., Reference Boateng, Doku, Enyan, Owusu, Aboh, Kodom, Ekumah, Quansah, Boamah, Obiri-Yeboah, Nsabimana, Jansen and Armah2021).
Marital status
Marital status was examined in two studies, all of which reported consistent results. One study found that living without a regular partner was significantly associated with increased odds of anxiety symptoms (Opoku Agyemang et al., Reference Opoku Agyemang, Ninonni, Bennin, Agyare, Gyimah, Senya, Birikorang, Quarshie, Baddoo, Addo and Obiri-Yeboah2022b), whereas the other study found that being married or in a union was significantly associated with lower levels of anxiety symptoms (Boateng et al., Reference Boateng, Doku, Enyan, Owusu, Aboh, Kodom, Ekumah, Quansah, Boamah, Obiri-Yeboah, Nsabimana, Jansen and Armah2021).
Economic domain
Economic factors were examined in two studies. One study found that high income was significantly associated with lower odds of anxiety symptoms (Amu et al., Reference Amu, Osei, Kofie, Owusu, Bosoka, Konlan, Kim, Orish, Maalman, Manu, Parbey, Saah, Mumuni, Appiah, Komesuor, Ayanore, Amenuvegbe, Kim, Jung, Adjuik, Tarkang, Alhassan, Donkor, Zottor, Kweku, Amuna, Kim and Gyapong2021), whereas the other study reported that anticipating better remuneration was significantly associated with higher odds of anxiety symptoms (Saah et al., Reference Saah, Amu and Kissah-Korsah2021).
Neighbourhood domain
One study examined this domain and found that living in an urban environment was associated with higher odds of anxiety symptoms compared to living in rural and semi-urban environments (Omuojine et al., Reference Omuojine, Nguah, Ayisi-Boateng, Sarfo and Ovbiagele2022).
Social and cultural domain
Three studies examined the association between educational attainment and anxiety symptoms. Among these, two studies found that having no formal education was significantly associated with higher levels of anxiety symptoms (Amu et al., Reference Amu, Osei, Kofie, Owusu, Bosoka, Konlan, Kim, Orish, Maalman, Manu, Parbey, Saah, Mumuni, Appiah, Komesuor, Ayanore, Amenuvegbe, Kim, Jung, Adjuik, Tarkang, Alhassan, Donkor, Zottor, Kweku, Amuna, Kim and Gyapong2021; Opoku Agyemang et al., Reference Opoku Agyemang, Ninonni, Bennin, Agyare, Gyimah, Senya, Birikorang, Quarshie, Baddoo, Addo and Obiri-Yeboah2022b). One study found that having a master’s degree was significantly associated with decreased odds of anxiety symptoms compared to a diploma (Opoku Agyemang et al., Reference Opoku Agyemang, Ninnoni and Enyan2022a). A study examining the interaction between male gender and education found that males without formal education had higher odds of experiencing anxiety symptoms than those with tertiary education (Opoku Agyemang et al., Reference Opoku Agyemang, Ninonni, Bennin, Agyare, Gyimah, Senya, Birikorang, Quarshie, Baddoo, Addo and Obiri-Yeboah2022b).
Social determinants of mental health associated with depressive symptoms
Twelve cross-sectional studies (N = 6,223) reported one or more proximal SDOMH associated with depressive symptoms (see Table 2). All studies performed multivariable statistical analysis, with adjustment for covariates. None of the studies examined environmental events and neighbourhood factors associated with depressive symptoms and SDOMH associated with depressive disorders.
Demographic domain
A total of six cross-sectional studies examined demographic factors that were categorised into five distinct subdomains: age, ethnicity, gender, marital status and religion.
Age
One study found that increasing age was significantly associated with higher odds of depressive symptoms, particularly among people living with HIV (Nutor et al., Reference Nutor, Alhassan, Thompson, Asakitogum, Duah, Ritchwood, Nkosi, Klaas, Agyemang and Gyamerah2024).
Ethnicity
The association between ethnicity and depressive symptoms was examined in two studies. One study found that Guans had the lowest odds of experiencing depressive symptoms compared to Akans, Ewes, Mole-Dagbanis and other unspecified ethnic groups (Amu et al., Reference Amu, Osei, Kofie, Owusu, Bosoka, Konlan, Kim, Orish, Maalman, Manu, Parbey, Saah, Mumuni, Appiah, Komesuor, Ayanore, Amenuvegbe, Kim, Jung, Adjuik, Tarkang, Alhassan, Donkor, Zottor, Kweku, Amuna, Kim and Gyapong2021). The other study found that waiters who were Ewe, Ga-Adangme, Mole Dagbani, and identified with other ethnicities had increased odds of experiencing depressive symptoms compared to Akans (Saah et al., Reference Saah, Amu and Kissah-Korsah2021).
Gender
Gender was examined in four studies, all of which reported consistent results. Among these, two studies found that female gender was significantly associated with increased odds of depressive symptoms (Akpalu et al., Reference Akpalu, Yorke, Ainuson-Quampah, Balogun and Yeboah2018; Saah et al., Reference Saah, Amu and Kissah-Korsah2021; Opoku Agyemang et al., Reference Opoku Agyemang, Ninonni, Bennin, Agyare, Gyimah, Senya, Birikorang, Quarshie, Baddoo, Addo and Obiri-Yeboah2022b). Another study found that men living with HIV had increased odds of experiencing depressive symptoms compared to those without it (Nutor et al., Reference Nutor, Alhassan, Thompson, Asakitogum, Duah, Ritchwood, Nkosi, Klaas, Agyemang and Gyamerah2024).
Marital status
Marital status was examined in two studies, all of which reported consistent results. One study found that, on average, adults who were married had decreased odds of experiencing depressive symptoms compared to those who were unmarried, divorced, widowed or separated (Akpalu et al., Reference Akpalu, Yorke, Ainuson-Quampah, Balogun and Yeboah2018). The other study found that being single was significantly associated with increased odds of depressive symptoms (Nakua et al., Reference Nakua, Amissah, Tawiah, Barnie, Donkor and Mock2023).
Religion
One study found that being a non-Christian was significantly associated with increased odds of depressive symptoms (Kugbey et al., Reference Kugbey, Nortu, Akpalu, Ayanore and Zotor2018).
Economic domain
Six cross-sectional studies examined the association between economic factors and depressive symptoms. Economic factors were categorised into two sub-domains: employment-related factors and income.
Employment-related factors
Employment-related factors were examined in three studies. One study found that job loss and self-employment were significantly associated with increased odds of depressive symptoms (Adu et al., Reference Adu, Wallace, Lartey, Arthur, Oteng, Dwomoh, Owusu-Antwi, Larsen-Reindorf and Agyapong2021). Another study found that anticipating better remuneration was significantly associated with increased odds of depressive symptoms (Saah et al., Reference Saah, Amu and Kissah-Korsah2021). One study found that there was no discernible association between occupation and depressive symptoms (Amu et al., Reference Amu, Osei, Kofie, Owusu, Bosoka, Konlan, Kim, Orish, Maalman, Manu, Parbey, Saah, Mumuni, Appiah, Komesuor, Ayanore, Amenuvegbe, Kim, Jung, Adjuik, Tarkang, Alhassan, Donkor, Zottor, Kweku, Amuna, Kim and Gyapong2021).
Income
Income was examined in four studies, all of which reported consistent results. One study found that low income (i.e., ≤ GH₵1,500.00, equivalent to $141.6 USD) was significantly associated with increased odds of depressive symptoms (Opoku Agyemang et al., Reference Opoku Agyemang, Ninnoni and Enyan2022a). Similarly, another study found that low monthly household income (i.e., GH₵ 50.00, equivalent to 4.71 USD) was associated with higher odds of depressive symptoms; however, only with borderline significance (Ofori-Atta et al., Reference Ofori-Atta, Reynolds, Antwi, Renner, Nichols, Lartey, Amissah, Tettey, Alhassan, Ofori, Catlin, Gan, Kyriakides and Paintsil2019). One study found that high income (> GH₵1,000.00, equivalent to $94.4 USD) was significantly associated with lower odds of depressive symptoms (Amu et al., Reference Amu, Osei, Kofie, Owusu, Bosoka, Konlan, Kim, Orish, Maalman, Manu, Parbey, Saah, Mumuni, Appiah, Komesuor, Ayanore, Amenuvegbe, Kim, Jung, Adjuik, Tarkang, Alhassan, Donkor, Zottor, Kweku, Amuna, Kim and Gyapong2021). One study found that low wealth was significantly associated with increased odds of depressive symptoms (Nakua et al., Reference Nakua, Amissah, Tawiah, Barnie, Donkor and Mock2023).
Social and cultural domain
Seven cross-sectional studies examined social and cultural factors associated with depressive symptoms. These factors were categorised into three sub-domains: educational attainment, living alone and social support and traumatic experiences.
Educational attainment
Educational attainment was variably associated with depressive symptoms across five studies. Among these, one study found that master’s degree holders had increased odds of experiencing severe depressive symptoms compared with diploma and bachelor’s degree holders (Opoku Agyemang et al., Reference Opoku Agyemang, Ninnoni and Enyan2022a). Similarly, another study found that adults with secondary education had increased odds of experiencing depressive symptoms compared to those without formal education (Nutor et al., Reference Nutor, Alhassan, Thompson, Asakitogum, Duah, Ritchwood, Nkosi, Klaas, Agyemang and Gyamerah2024). However, two studies found that higher educational attainment was significantly associated with decreased odds of depressive symptoms. Among these two studies, one found that adults with tertiary education had decreased odds of experiencing depressive symptoms compared to those without formal education (Amu et al., Reference Amu, Osei, Kofie, Owusu, Bosoka, Konlan, Kim, Orish, Maalman, Manu, Parbey, Saah, Mumuni, Appiah, Komesuor, Ayanore, Amenuvegbe, Kim, Jung, Adjuik, Tarkang, Alhassan, Donkor, Zottor, Kweku, Amuna, Kim and Gyapong2021). The other study found that formal education and English reading ability were significantly associated with decreased odds of depressive symptoms (Kugbey, Reference Kugbey2022). One study examining the interaction between gender and education found that males, particularly those living with HIV without formal education, had increased odds of experiencing depressive symptoms compared to those with tertiary education (Opoku Agyemang et al., Reference Opoku Agyemang, Ninonni, Bennin, Agyare, Gyimah, Senya, Birikorang, Quarshie, Baddoo, Addo and Obiri-Yeboah2022b).
Living alone and social support
Two studies found that lack of social support (Asante and Andoh-Arthur, Reference Oppong Asante and Andoh-Arthur2015) and high social support (Nutor et al., Reference Nutor, Alhassan, Thompson, Asakitogum, Duah, Ritchwood, Nkosi, Klaas, Agyemang and Gyamerah2024) were significantly associated with increased odds of depressive symptoms. One study found that living alone was significantly associated with higher odds of depressive symptoms (Kugbey et al., Reference Kugbey, Nortu, Akpalu, Ayanore and Zotor2018).
Traumatic experiences
One study found that traumatic experiences, such as being beaten by an intimate partner, childhood physical and sexual abuse, and forced sex, were significantly associated with higher odds of depressive symptoms (Asante and Andoh-Arthur, Reference Oppong Asante and Andoh-Arthur2015).
Discussion
Pooled point prevalence of anxiety disorders and symptoms, depressive disorders and symptoms, and symptoms of psychological distress was 40.3%, 33.0% and 36.7%, respectively, highlighting a significant mental health burden among adults in Ghana. Reviews conducted in other LMICs have reported varying point prevalence rates of anxiety and depression disorders and symptoms among adults (Bello et al., Reference Bello, Kannan, Chutiyami, Salihu, Cheong, Miller, Pun, Muhammad, Mahmud, Jalo, Ali, Kolo, Sulaiman, Lawan, Bello, Gambo and Winser2022; Kaggwa et al., Reference Kaggwa, Najjuka, Bongomin, Mamun and Griffiths2022; Opio et al., Reference Opio, Munn and Aromataris2022). The point prevalence of anxiety disorders (20.2%) and depressive disorders (21.2%) reported in a review from Uganda (Opio et al., Reference Opio, Munn and Aromataris2022) was lower than the estimates observed in our review. Similarly, another review from Uganda reported a slightly lower point prevalence of depressive disorders and symptoms (30.2%) (Kaggwa et al., Reference Kaggwa, Najjuka, Bongomin, Mamun and Griffiths2022), compared to our findings. In contrast, a review focusing on the African continent reported higher prevalence rates for anxiety (47%) and depressive symptoms (48%). Potential reasons for discrepancies in prevalence estimates may include the small number of studies on anxiety (5) and depressive disorders (19), and differences in populations studied (i.e., adults and children) in the two reviews from Uganda (Kaggwa et al., Reference Kaggwa, Najjuka, Bongomin, Mamun and Griffiths2022; Opio et al., Reference Opio, Munn and Aromataris2022) compared with our review, and the potential impact of the COVID-19 pandemic, which may have elevated prevalence rates across Africa (Bello et al., Reference Bello, Kannan, Chutiyami, Salihu, Cheong, Miller, Pun, Muhammad, Mahmud, Jalo, Ali, Kolo, Sulaiman, Lawan, Bello, Gambo and Winser2022). Comparisons with other reviews are also limited due to variations in inclusion criteria, population characteristics and methodologies. The high degree of heterogeneity found across studies, predominant use of self-reported screening tools compared to diagnostic interviews, and high risk of bias identified in quality domains related to sample coverage, sampling methods, condition measurement, and response rate warrant a cautious interpretation of our findings.
Geographical location was a significant moderator of the prevalence of anxiety disorders and symptoms, and prevalence of depressive disorders and symptoms. Higher prevalence rates were reported in studies conducted in the Southern regions of Ghana, particularly Greater Accra and Ashanti region, whereas prevalence studies were limited or not available in the Northern regions of Ghana (e.g., Upper East region). Variability in regional coverage of prevalence data aligns with mental health service distribution in Ghana, which is skewed towards the Southern regions of Ghana, with limited service availability in the Northern regions (Eaton and Ohene, Reference Eaton and Ohene2016; Mwangi et al., Reference Mwangi, Sakyi, Ae-Ngibise, Lund and Weobong2023). The Northern regions face socioeconomic challenges attributable to factors including climate change, ethnic conflict, food insecurity, and natural disasters, which may contribute to a higher mental health burden. However, limited research, particularly from the Northern regions of Ghana, limits our understanding of the mental health needs of those residing in these regions (Eaton and Ohene, Reference Eaton and Ohene2016; Mwangi et al., Reference Mwangi, Sakyi, Ae-Ngibise, Lund and Weobong2023). We also found that the point prevalence of anxiety disorders and symptoms (54.1%), and the point prevalence of depressive disorders and symptoms (37.7%) were higher in studies conducted before 2020 than those conducted from 2020 onwards, consistent with trends observed in other reviews (Cai et al., Reference Cai, Chen, Zhang, Lam, Si, Liu, Zheng, Su, Cheung, Jackson, Ungvari, Ren, Li, X-H and Xiang2024). However, some studies reporting the prevalence of anxiety (four studies) and depressive (nine studies) disorders and symptoms did not report time periods for recruitment and data collection, limiting our ability to draw any definitive conclusions about prevalence rates over time. Findings highlight the need to strengthen the reporting practices of prevalence research to enable comparisons of prevalence estimates over time.
Included studies predominantly used self-report screening tools and clinical cut-offs instead of clinician-administered diagnostic interviews. Clinician-administered diagnostic interviews, widely considered the “gold standard” method of assessing anxiety and depressive disorders, often yield lower prevalence estimates than those obtained using clinical cutoffs on self-report screening tools. However, clinician-administered diagnostic interviews tend to be expensive and time-intensive to use for prevalence research or population-wide surveys (Brown et al., Reference Brown, Eisner, Walker, Tomlinson, Fearon, Dunne, Valdebenito, Hughes, Ward, Sikander, Osafo, Madrid, Baban, Van Thang, Fernando and Murray2021). In Ghana, the use of self-report screening tools has been found to be more feasible for large-scale prevalence studies due to the limited number of trained professionals and funding constraints (Agyapong et al., Reference Agyapong, Osei, Farren and McAuliffe2015). Yet, self-report screening tools vary in sensitivity and specificity, and may have contributed to higher prevalence estimates reported in our review (Jia et al., Reference Jia, Zhou, Xiang, Hu and Cao2024). Further, cut-off points used across studies commonly vary (Zimmerman, Reference Zimmerman2024). In our review, studies using the same self-report screening tool used different cut-offs. For example, studies using the PHQ-9 used cut-offs ranging from ≥3 (three studies) to ≥10 (three studies). The use of culturally adapted and validated self-report screening tools and cut-offs to measure the prevalence of anxiety and depression disorders and symptoms would improve the accuracy and comparability of prevalence estimates in Ghana and across reviews (Deng et al., Reference Deng, Zhou, Hou, Silver, Wong, Chang, Drakos, Zuo and Huang2021; Nielsen-Scott et al., Reference Nielsen-Scott, Fellmeth, Opondo and Alderdice2022).
Subgroup analysis showed that the presence of a chronic physical condition was a significant moderator of the point prevalence of anxiety disorders and symptoms, with higher rates observed among adults with a chronic physical condition (57.3%) than those without (32.2%). This finding is consistent with previous literature highlighting the disproportionate burden of chronic physical health conditions in LMICs, and their co-occurrence with higher rates of anxiety disorders and symptoms, particularly among adults living with breast cancer (Kyei, Reference Kyei2018; Bello et al., Reference Bello, Kannan, Chutiyami, Salihu, Cheong, Miller, Pun, Muhammad, Mahmud, Jalo, Ali, Kolo, Sulaiman, Lawan, Bello, Gambo and Winser2022; Rohwer et al., Reference Rohwer, Toews, Uwimana-Nicol, Nyirenda, Niyibizi, Akiteng, Meerpohl, Bavuma, Kredo and Young2023). Higher rates of anxiety disorders and symptoms may pose a significant challenge to the management of chronic physical conditions, interfering with healthcare utilisation, treatment outcomes and quality of life (Kugbey, Reference Kugbey2022). Findings suggest a need for regular screening of anxiety disorders and symptoms as part of routine care to inform treatment decisions and appropriate referrals for adults living with chronic physical conditions in Ghana.
Overall, in relation to SDOMH, we found that demographic, economic, social and cultural factors were more frequently studied compared to environmental events and neighbourhood factors. Most evidence was found in the demographic domain, where increasing age, younger age, female gender and marital status were found to be significant predictors of higher odds of anxiety and depressive symptoms in adults, consistent with previous reviews (Silva et al., Reference Silva, Loureiro and Cardoso2016; Lund et al., Reference Lund, Brooke-Sumner, Baingana, Baron, Breuer, Chandra, Haushofer, Herrman, Jordans, Kieling, Medina-Mora, Morgan, Omigbodun, Tol, Patel and Saxena2018). Evidence on social and cultural factors, including childhood physical and sexual abuse, forced sex, intimate partner violence, and educational attainment and their association particularly with depressive symptoms was limited (Asante and Andoh-Arthur, Reference Oppong Asante and Andoh-Arthur2015; Kugbey, Reference Kugbey2022). The review identified patterns consistent with the social gradient in mental health, whereby job loss, lower wealth, low educational attainment, low income and low social support were associated with increased odds of anxiety and depressive symptoms, consistent with previous research (Alegría et al., Reference Alegría, NeMoyer, Falgàs Bagué, Wang and Alvarez2018; Lund et al., Reference Lund, Brooke-Sumner, Baingana, Baron, Breuer, Chandra, Haushofer, Herrman, Jordans, Kieling, Medina-Mora, Morgan, Omigbodun, Tol, Patel and Saxena2018). Some studies found that anticipated increase in remuneration, higher educational attainment, high social support and self-employment were associated with higher odds of depressive symptoms in adults, potentially suggesting that SDOMH may operate through complex and context-dependent pathways that cross-sectional studies may not fully capture (Lund et al., Reference Lund, Brooke-Sumner, Baingana, Baron, Breuer, Chandra, Haushofer, Herrman, Jordans, Kieling, Medina-Mora, Morgan, Omigbodun, Tol, Patel and Saxena2018). Importantly, the review found significant gaps regarding neighbourhood factors and environmental events potentially associated with anxiety and depressive symptoms. Research on neighbourhood factors was scarce, with only one study reporting that living in an urban environment was associated with an increased odds of anxiety symptoms (Omuojine et al., Reference Omuojine, Nguah, Ayisi-Boateng, Sarfo and Ovbiagele2022). This finding is consistent with previous research reporting that urban living exposes residents to anxiogenic factors, such as high stress levels, noise pollution, violence and reduced social cohesion, compared to rural and semi-urban environments (Silva et al., Reference Silva, Loureiro and Cardoso2016; Lund et al., Reference Lund, Brooke-Sumner, Baingana, Baron, Breuer, Chandra, Haushofer, Herrman, Jordans, Kieling, Medina-Mora, Morgan, Omigbodun, Tol, Patel and Saxena2018). None of the reviewed studies examined the association between environmental events, including climate change, forced migration, natural disasters and anxiety and depressive disorders and symptoms. Findings should be interpreted cautiously, given that few studies explored the same SDOMH, and our understanding of both the interaction between SDOMH and how SDOMH contributes to the varying burden of anxiety and depressive symptoms is limited.
Strengths and limitations
This review has several strengths. We utilised a comprehensive electronic search strategy, peer reviewed following the PRESS guideline to minimise the risk of missing relevant studies. We adhered to quality standards informed by the JBI critical appraisal checklist and PRISMA checklist, with screening steps conducted by two independent reviewers. We included studies of chronic physical health populations, recognising that mental health difficulties often co-occur with physical health conditions. We explored SDOMH associated with anxiety and depressive disorders and symptoms, which are relevant for achieving the SDGs (e.g., SDG 1 [ending poverty], SDG 5 [gender equality], SDG 8 [decent work and economic growth], SDG 9 [industry, innovation and infrastructure], and SDG 10 [reducing inequalities], and informing strategies to reduce the mental health burden among adults.
Limitations of the review included substantial heterogeneity arising from variations in study population and assessment methods, limiting direct comparison with other reviews. While sources of heterogeneity were examined via subgroup analysis, other potential moderators of prevalence estimate, for example, mean age and income, were not examined via meta-regression due to inconsistent reporting. Most studies used different self-reported screening tools with varied cut-offs rather than diagnostic interviews to measure the prevalence of anxiety and depressive disorders, which may have skewed prevalence estimates. Another major limitation of the review is the over-reliance of studies on cross-sectional designs (100%), limiting causal inference and theorisation of the direction and importance of relative SDOMH over time. Most of the reviewed studies examined SDOMH as isolated factors without examining the complex interactions among SDOMH, including how proximal SDOMH interact with distal SDOMH, or specifying pathways through which SDOMH influence mental health outcomes. Qualitative studies were excluded, limiting an in-depth exploration of the perspectives of adults in Ghana on SDOMH potentially associated with anxiety and depressive disorders and symptoms, which may have provided important insights to inform future intervention development.
Implications for clinical practice and policy
Current evidence, although limited and largely cross-sectional, suggests a potential association between proximal SDOMH and anxiety and depressive symptoms in adults. Addressing the adverse impacts of SDOMH and increasing access to mental health services via the NHIS can facilitate early diagnosis and treatment, and reduce health inequities. A range of intervention study designs (e.g., randomised controlled trials) are required to examine the effect of individual-level and population-level interventions, such as awareness campaigns, cash transfers (e.g., Livelihood Empowerment Against Poverty (LEAP programme), neighbourhood regeneration programmes, social prescribing, trauma-informed therapies and vocational support, on adult mental health outcomes (Kirkbride et al., Reference Kirkbride, Anglin, Colman, Dykxhoorn, Jones, Patalay, Pitman, Soneson, Steare, Wright and Griffiths2024). Importantly, Ghana’s Mental Health Policy 2019–2030 (Government of Ghana, 2018) makes little to no explicit reference to SDOMH, with socioeconomic factors mentioned only once. There is an urgent need for policymakers in Ghana to revise existing mental health policies and programmes to explicitly incorporate SDOMH considerations and allocate adequate financial resources for their implementation. In alignment with resolution WHA74.16 (World Health Organization, 2024), which calls on member states to monitor and act on SDOMH. It is crucial that the Government of Ghana develops robust indicators to track SDOMH and the mental health status of diverse populations in Ghana. Further, clinical monitoring, documentation and interventions addressing SDOMH are gaining international acceptance (Andermann, Reference Andermann2018), and more research is required to evaluate the impact, acceptability, effectiveness and feasibility of these practices within the Ghanaian health context.
Implications for research
Over-reliance on self-report screening tools that have been validated for adult populations in other contexts, without adaptation to the Ghanaian context, risks overlooking culturally specific expressions of symptoms of anxiety, depression and distress (e.g., brain fatigue and tension in the head) (Ali et al., Reference Ali, Ryan and Silva2016; Desai and Chaturvedi, Reference Desai and Chaturvedi2017). Further, globally recommended cut-offs may not be applicable to LMIC populations, and their use without adaptation to the local context may lead to inaccuracies in prevalence estimates (Ali et al., Reference Ali, Ryan and Silva2016). Therefore, future research should prioritise the cultural adaptation and validation of clinician-administered diagnostic interviews and self-report screening tools to ensure accurate assessment of anxiety and depressive symptoms in adult populations in Ghana.
We assessed publication bias despite contention around its appropriateness for systematic reviews of prevalence, that is, as prevalence studies do not test for statistical significance, the notion of publication bias (e.g., statistically significant studies are more likely to be published) may not be applicable to prevalence studies (Peters et al., Reference Peters, Sutton, Jones, Abrams and Rushton2006; Borenstein, Reference Borenstein2019). Future research should investigate the advantages and disadvantages of assessing publication bias in prevalence studies, as well as consider other sources of potential bias (e.g., omitted variable bias and Neyman bias), which may be particularly relevant to prevalence research (Tripepi et al., Reference Tripepi, Jager, Dekker, Wanner and Zoccali2008). Future studies should prioritise longitudinal, multilevel and integrative study designs that can effectively capture the complex interactions between proximal and distal SDOMH, and their relative importance over time.
Conclusions
Anxiety and depressive symptoms are common among adults in Ghana. Social determinants of mental health, including educational attainment, female gender, low income, urban environment and traumatic experiences, may be associated with the prevalence of anxiety and depressive symptoms. While our findings indicate a potentially significant mental health burden in Ghana, high levels of heterogeneity and over-reliance on self-reported screening tools suggest a need for caution in interpreting prevalence estimates. Research training programs and financial resources are needed to support the conduct of high-quality prevalence research that can guide clinical interventions and policy planning.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2025.10122.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/gmh.2025.10122.
Data availability statement
All data are provided in the article and Supplementary Material.
Acknowledgements
The authors would like to thank Mattias Axén and Malin Barkelind, librarians at Uppsala University Library, for assisting with the electronic search strategy. The authors would also like to thank Alkistis Skalkidou at Uppsala University and Lene Lindberg at Karolinska Institute for peer reviewing the search strategy. We would like to thank Chelsea Coumoundouros for her support during the initial stages of this review.
Author contribution
Victoria Awortwe: Conceptualisation; methodology; validation; formal analysis; investigation; data curation; writing – original draft; writing – review and editing; visualisation; project administration. Febrina Maharani: Validation; formal analysis; investigation; data curation; writing – review and editing; visualisation. Meena Daivadanam: Conceptualisation; methodology; writing – review and editing; project administration; supervision. Samuel Adjorlolo: Methodology; writing – review and editing; supervision. Erik M. G. Olsson: Methodology; writing – review and editing; supervision. Louise von-Essen: Resources; writing – review and editing; funding acquisition. Vian Rajabzadeh: Validation; investigation; writing – review and editing. Joanne Woodford: Conceptualisation; methodology; validation; investigation; writing – review and editing; project administration; supervision.
Financial support
This work was supported by U-CARE, which is a strategic research environment funded by the Swedish Research Council (dnr 2009–1,093). This funding source had no role in the design of this review, its execution, analyses, interpretation or decision to submit results.
Competing interests
The authors declare none.
Ethics statement
No ethical approval was required as this review synthesised only publicly available data.




Comments
The Editor
Cambridge Prisms: Global Mental Health 11th May, 2025
Dear Editor,
Please find enclosed our manuscript which we would like to submit for publication as a review in Cambridge Prisms: Global Mental Health. The manuscript and author details are as follow:
Title: Prevalence and social determinants of anxiety and depressive disorders and symptoms among adults in Ghana: a systematic review and meta-analysis
Authors: Victoria Awortwe, Meena Daivadanam, Febrina Maharani, Samuel Adjorlolo, Erik MG Olsson, Louise Von Essen, Vian Rajabzadeh, and Joanne Woodford
Our systematic review examines the prevalence and social determiants of anxiety and depressive disorders and symptoms among adults in Ghana, with a focus on proximal and distal demographic, economic, environmental, neigbhourhood, and socio-cultural factors linked to the sustainable development goals, that contribute to inequities in mental health outcomes in this population. Given the increasing recognition of the role of social determinants of mental health in the reduction of population-level burden of mental disorders, this work offers insights relevant to discussions on mental health disparities, particularly in low-and middle-income country (LMIC) setting.
While much of the existing literature emphasises biological and psychological determinants, our review highlights the critical yet underexplored role of social determinants of mental health. Additionally, the review discusses important methodological challenges in mental health research, including:
(1) The overreliance on self-reporting screening tool (with varying cutoffs) rather than diagnostic interviews and its implications for prevalence estimates
(2) The need for culturally validated mental health assessment tools to improve measurement accuracy and comparability
(3) The uneven distribution of studies across regions, limiting a comprehensive understanding of mental health burdens
The review addresses broader global challenges in mental health research. Many of the methodological issues raised such as the reliance on self-report tools and the importance of culturally appropriate assessments are common across LMICs and some high-income settings with diverse populations. By discussing these challenges, the review contributes to ongoing international debates on improving mental health measurement, addressing mental health disparities, and integrating social determinants into mental health policy and clinical practice.
We believe that findings from this paper would be of interest to the Government of Ghana whose efforts to improve the mental wellbeing via the recently revised Mental Health policy has been hindered by the absence of a comprehensive prevalence and social determinants of mental health data. Further, our findings would be of interest to a range of international audiences, including other researchers, clinicians, and policy makers.
Due to the scope and depth of the literature covered, the current version of the manuscript exceeds the journal’s word limit by approximately 500 words. We have made substantial efforts to condense the content. We also sent an email to the editorial office to ascertain whether the journal might allow some flexibility with the word count in this case. We would be grateful for your consideration and are happy to revise further if needed. We confirm that this manuscript has not been published elsewhere and is not under consideration by another journal. All authors have read and approved the manuscript. All communication should be directed to the corresponding author, details as follows:
Corresponding author & contact details: Victoria Awortwe, PhD student, Department of Women’s and Children’s Health, Uppsala University
E-mail: victoria.awortwe@uu.se
Mobile: +46769782339
Thank you in advance for your consideration. We look forward to hearing from you at your earliest convenience.
Yours sincerely,
Mrs. Victoria Awortwe