Case presentation
We describe a case of a 5-month-old infant with a large perimembranous ventricular septal defect, referred for elective surgical repair. Pre-operative electrocardiogram showed normal sinus rhythm, right axis deviation, and right ventricular hypertrophy. Pre-operative transthoracic echocardiogram showed large perimembranous ventricular septal defect with low velocity bidirectional shunting (left to right in systole), qualitatively normal right ventricular size, wall thickness, and systolic function; and a tricuspid regurgitation jet estimating the right ventricular systolic pressure of 58 mmHg. Normal origins of the right and left main coronary arteries were demonstrated by two-dimensional imaging and colour Doppler pattern. The repair was without technical complications; however, there were peaked T-waves upon coming off cardiopulmonary bypass. Post-operative transesophageal echocardiogram showed mild-to-moderate reduction in systolic function that progressively improved during the scan. Post-operative 12-lead electrocardiogram demonstrated right bundle branch block with abnormal superior right axis deviation and large T waves in all leads without pathologic ST-elevations or new Q waves (Figure 1a).

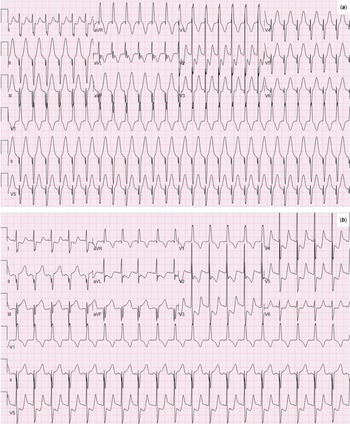
Figure 1. Immediate post-operative ECG with peaked T waves, RAD, and RBBB (a) POD 1 ECG with ST-elevations in leads II, III, augmented vector foot (aVF), and ST-depressions in V2–5 (b).
On post-operative day 1, the patient remained intubated and was hemodynamically stable on milrinone and low-dose epinephrine infusions. She developed ST-elevations in leads II, III, aVF, and ST-depressions in V2–5 on her 12-lead electrocardiogram (Figure 1b). Transthoracic echocardiogram showed severe left ventricular systolic dysfunction with hypokinesis of basal, mid-inferior, and inferolateral wall segments of the myocardium. Early morning on post-operative day 2, she had a brief bradycardic event with positioning for chest X-ray responsive to a dose of epinephrine. She was subsequently transported for urgent catheterisation.
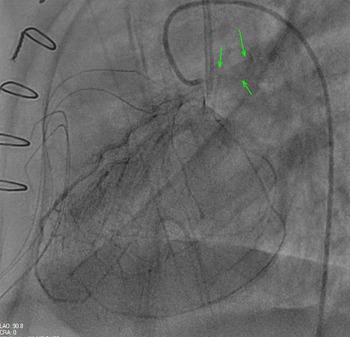
Selective coronary injection of the left coronary artery demonstrated a normal course of the left anterior descending artery with a left-dominant coronary system. There was retrograde filling of the left circumflex artery appreciated. The left circumflex; origin could not be definitively identified by direct injection, though levophase demonstrated late filling of the main pulmonary artery without normal connection to the aortic root (Figure 2). The patient was transferred immediately from the catheterisation laboratory to the CT scanner with confirmation of anomalous origin of the circumflex coronary artery from the posterior aspect of the main pulmonary artery before returning to the ICU with referral for emergent coronary reimplantation.

Figure 2. Selective left coronary artery injection with 3.3 Fr JL1 catheter in lateral projection demonstrates a left-dominant coronary artery system, with the left anterior descending artery joining the left posterior descending artery. There is retrograde filling of the circumflex coronary artery with blush of contrast to the main pulmonary artery (green arrows).
While the operating room was being prepared, she developed hemodynamic instability with pulseless arrest responsive to one round of compressions and epinephrine administration. Once in the operating room, she developed pulseless arrest again with prompt initiation of cardiopulmonary bypass. The left circumflex artery was confirmed to originate from the posterior aspect of the main pulmonary artery, adjacent to the take-off of the right pulmonary artery, and was reimplanted in the posterior aspect of the ascending aorta. Despite reimplantation, the patient had ongoing ventricular dysfunction and returned to the ICU on veno-arterial extracorporeal membrane oxygenation.
The following morning, a left atrial vent was placed due to persistent cardiac dysfunction. The patient was transferred to a quaternary institution for higher level of care and ventricular assist consideration. Despite ongoing mechanical circulatory support, the patient ultimately expired following brain injury.
Discussion
Coronary arteries form with migration of the proepicardium to envelop the myocardium. The proepicardium thickens, preferentially over the atria and atrioventricular groove. As cells lose contact with the epicardial epithelium, they transition into mesenchymal cells and form channels that become the endothelium of coronary arteries. Reference Reese, Mikawa and Bader1 Coronary ostia are formed by capillary penetration of the aortic root. Anomalous coronary arteries occur due to failure of the capillary plexus surrounding the aorta and main pulmonary artery to penetrate the appropriate sites on the aorta. Reference Tomanek and Angelini2 For example, in anomalous left coronary artery from pulmonary artery, the capillary penetration occurs ectopically at the main pulmonary artery. Reference Reese, Mikawa and Bader1,Reference Tomanek and Angelini2
In one retrospective study of patients who underwent coronary angiography, coronary anomalies were present in 0.9% of paediatric patients. Reference Tuo3 However, in those with CHD, the risk of having coronary anomalies is higher, with some studies reporting up to 36% of patients with CHD having anomalous coronaries. Reference Taylor4 Moreover, variation in coronary artery anatomy is more common in patients who have left coronary dominance. Reference Eren5 Anomalous origin of coronary arteries can be fatal if unrecognised. Anomalous left coronary artery from pulmonary artery occurs in 1 in 300,000 live births, comprising 0.24–0.46% of infants with CHD. Reference George6 Anomalous left circumflex artery from pulmonary artery is furthermore rare, with very few cases reported in the literature.
The anomalous left circumflex artery in this case likely experienced a steal phenomenon from the main pulmonary artery with closure of the ventricular septal defect. Closure of the ventricular septal defect led to decreased pressure transmitted to the main pulmonary artery with removal of the left to right intracardiac shunt. Without forward driving pressure, there was no longer prograde flow from the left circumflex artery to the posterior wall of the heart. In addition, the myocardial bed was likely not adequately protected during cardiac arrest in the operating room. A single 20 mL/kg dose of cold blood Del Nido cardioplegia was injected into the aortic root, which is standard for low-risk, routine ventricular septal defect repairs. Ideally, it would flow through the left and right coronary arteries, reaching the left circumflex artery and offering protection to the posterior heart. Reference Carvajal7 However, given this patient’s unanticipated anatomy, cardioplegia may not have reached her left circumflex artery and thus her posterior wall was likely ischaemic for the duration of the repair once the ventricular septal defect patch was completed.
While isolated new right bundle branch block is not uncommon after surgical closure of ventricular septal defect, it is unusual to have new superior right axis deviation with right bundle branch block after a perimembranous ventricular septal defect closure if no other CHD lesions are present. This suggested injury to the left inferior/ and posterior fascicles of left and right bundle of the cardiac conduction system in our patient. Due to her left-dominant coronary system, this patient lost perfusion not only to her postero-lateral walls but also her inferior wall and posterior/inferior fascicle, showing what we now know was posterior myocardial infarction on electrocardiogram.
This case adds to the sparse literature on anomalous left circumflex artery from pulmonary artery. In the case of post-operative CHD repair with ventricular dysfunction out of proportion to the expected course, it is important to consider undiagnosed anomalous coronary anatomy in the differential diagnosis. Early recognition may be amenable to intervention and preclude an adverse outcome.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None.